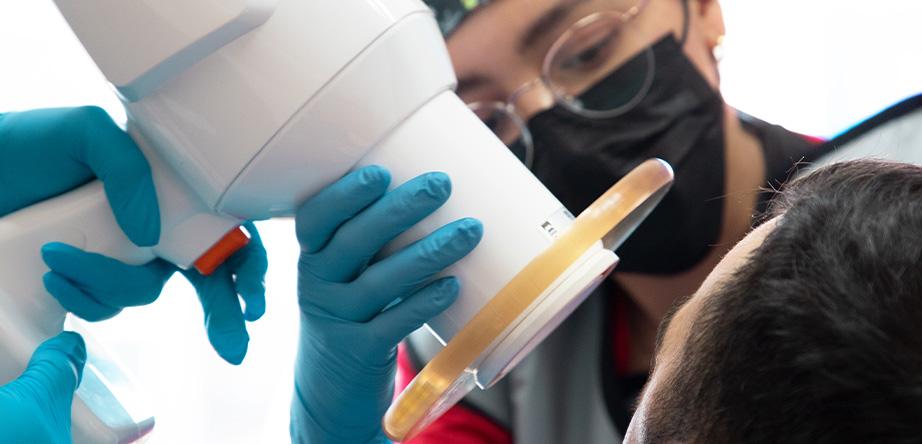
Stem Cells for Dental Implants

Stem Cells for Dental Implants are Here
You may not know this, but stem cells for dental implants can have a huge (and positive) impact on your smile! Since we only have two sets of teeth during our lifetime, losing a tooth as adults is really a problem.Over time, there have been dental solutions that seemed to be the final answer. As technology improves, dentistry needs to keep adopting new methods for tooth replacement. But before we jump into that subject, let me explain why stem cells for dental implants are even considered in the first place.
Tooth decay is often unnoticed in its early stages. And as you probably already noted, teeth problems get worse over time – if they’re left ignored. If your oral hygiene habits are not the greatest, they will lead – eventually- to tooth loss. However, there are times when it can’t be avoided, like accidents or age.
Getting dental implants to replace missing teeth has been a reality for some years now. But even this modern dental procedure keeps reinventing itself.
Dentures Were Once The Best Solution To Missing Teeth
The chance to restore a completely toothless jaw with artificial teeth has been out there since dentures got created. But dentures are a real challenge in the long run.One of the most concerning “side effects” of dentures is that they decrease the average strength of a human bite as years pass by. How can it happen exactly? Well, every time we need to take a bite, our body uses energy and applies force to cut a piece from this apple.

By the way, being a person with great jaw and bone structure doesn’t guarantee that you’ll be able to cut a piece from that apple. As it turns out, it’s not enough to have energy and power in our muscles. As Scientific American nicely put it: “…The limit of the bite is not determined by the muscles, but by the teeth themselves”. We are sorry to say but, weak teeth equal soft bites.
Weak teeth are not just teeth with cavities. They need to be strong from their roots, that’s why we rely on root canals to restore teeth. But their weakness can also come from underneath.
So, what’s underneath our teeth? There’s a membrane between our teeth and bones that should always be healthy. If it’s in good health condition it can work both as a cushion, and an anchor to our teeth.
To put it simply, teeth depend on this soft tissue to resist the stresses of chewing. Now, how can this be related to denture use? Everything, actually.
Time Affects our Bite
The strength of a human bite is actually an interesting subject. So much that, it has been tested in clinical trials. When we have our natural teeth, the average force of every bite is measured in the range of 150-250 psi (pounds per square inch of area). Whereas patients without teeth have a biting force of 50 psi or less. That’s a huge difference!When patients have worn their dentures for more than 15 years, the chewing strength is lost substantially. And that could also happen to anybody that waits too long to get their teeth reconstructed!
Delaying a visit to the dentist to get one or more missing teeth replaced will end up affecting the jawbone.
Your body knows when teeth are missing because it no longer feels pressure in that area. And since our bodies know the best way to optimize resources, it sets a limit on jawbone formation.
From this time on, bone formation where teeth used to be will be considered as “surplus production”. The result? Bone loss or resorption following a tooth extraction.
These changes are important, but they often pass unnoticed. There’s one thing that most patients do talk about. It’s the fear of having food restrictions with the dental treatment of their choice. And sadly, food restrictions are common among patients with dentures, and also between those with few or no teeth at all.
Healthy Teeth are Linked to Good Nutrition
People who are missing teeth and wear dentures tend to avoid raw vegetables and prefer food that’s easier to chew.As one study points out, denture wearers usually modify their diet in two ways: by progressively rejecting food that’s hard to chew like meat, fruits, and vegetables. And by changing how they cook, so that food texture gets altered.
Likewise, when food is not properly chewed, fewer nutrients are obtained from it. Unfortunately, all of this may lead to malnutrition.
It appears that avoiding certain foods is common among elderly people and those who are missing teeth.
We believe (and we hope you agree with us at this point) that besides improving the appearance and giving a great boost of confidence, replacing missing teeth enhances the nutritional status and health of people.
Dental Implants Replace Missing Teeth
One of the best solutions for teeth replacement is found in dental implants. They can restore a completely toothless jaw, they can even restore the same chewing force as natural teeth!However, in order for them to work, the final prosthesis needs to be firmly anchored into the jawbone, just as teeth roots are. That’s why implant screws are usually made of titanium, so they can mimic strong teeth roots. They fix the implants all the way to the bone.
But, have you ever wondered what happens when there’s not enough bone? You know, to firmly support an implant. Well, dentists have come up with different solutions for that.
Having poor bone quality doesn’t necessarily mean that you’re not a candidate for implants.
Bone Grafting
Bone grafting and implants are usually done together, it gives a new opportunity to promote bone growth in that location. In fact, increasing bone thickness is really common in Dentistry. We are going to mention four different techniques usually applied:Bone Graft. To increase bone density, bone flakes derived from non-human sources are grafted into the jawbone.
Sinus Lift. This surgery adds bone grafting material in the upper jawbone.
Onlay Graft. It uses bone from the patient’s own body and transfers it to the jawbone, where it is left to heal.
Synthetic Bone Graft Substitutes. Whether it’s in the form of gel, powder, putty, and chips, these substitutes are laid on top of the existing bone.
Regardless of the technique, the usual wait time for the grafted material to integrate with the surrounding bone is between 4-9 months. In the end, the bone should be ready to support a dental implant.
Innovations In Dental Implants
Cultivating Bone TissueBone grafting has proven to be effective and gives predictable results. There are some drawbacks though. The aforementioned methods are seen as time-consuming and there are times when the bone is not able to grow at the desired volume.
As we mentioned before, a dental implant is a modern dental procedure that keeps reinventing itself.
One of the pioneers in this field is Prof. Dr. Ralf Gutwald, from the University of Freiburg, in Germany. He and his team have started to cultivate bone tissue in vitro.
The process resembles that of the Onlay graft. They start by removing a small amount of bone tissue from the patient’s own body. But instead of placing it straight into the jawbone, it’s cultivated in the lab to let bone-producing cells develop and do their job.
Traditional Bone grafting procedures take from 4-9 months, whereas this method only takes two months.
After this time, the newly formed tissue is inserted into the jawbone. There it integrates, and finally becomes part of the bone itself.
Stem Cells Can Regenerate Jawbone
Now, this is a state-of-the-art method! Scientists have found a way to use the patient’s own stem cells to regenerate the jawbone.They found a protein that can get injected into the muscles to attract stem cells, that in turn produce bone.
This method can get replicated on clinical studies, still, scientists decided to do things the opposite way around: by bringing stem cells into the jawbone.
The way is done is fairly simple. Stem cells are removed from the bone marrow and get mixed with bone grafting material. This mixture is applied directly in the patient’s body, and bone forms in the area.
In just 4 months a patient’s jaw can have 30% more bone volume. What’s even greater is that with this method, new blood vessels also form, giving more nutrients and vitality to the area!
Stem Cells for Dental Implants
Given that our body already uses stem cells to replenish other cells, it was just a matter of time before we could understand how that process really works, so we could begin to replicate it.As you can see, dentistry has found methods to harness the benefits of stem cells for dental implants and mouth restoration.
Being able to treat a patient that just a few weeks ago had low bone density is quite amazing! The chance to place implants with a minimum time between stages surely gives many benefits to patients.
Biologics For a Faster Healing Well-equipped dental offices can always offer treatment options. Luckily, patients with gum disease have the option to get treated quicker than ever before.
Dentists today can guide the regeneration of bone and soft tissues to save and preserve the tooth. At other times, this regeneration is needed to guarantee implant attachment.
There are two different methods for this, the lab-made and the natural way.
The most preferred lab-made method is called EMD or enamel matrix derivative. EMD has become the standard for gum disease regeneration. Emdogain, its commercial form, is a gel applied during surgery.
Emdogain is backed by Straumann’s commitment to science. It’s a great protein mix that regulates inflammation and has an antimicrobial effect.
Among the natural ones, L-PRF is the most popular. It stands for leukocyte platelet-rich fibrin. It’s the most simple and economic natural method used in regenerative dentistry. However, experienced dentists prefer L-PRF for a simple reason. Because it gives a high success rate on bone and tissue regeneration.
L-PRF treatment only needs about four small vials of blood taken from the arm. Don’t worry, getting this tiny amount of blood drawn takes only a few minutes and is actually painless. This sample is placed in a special centrifuge that spins rapidly to create a clotted fibrin. At the end, the clot forms a matrix, which is like a biological glue.
The “glue” works just as a surgical Band-Aid. It’s a great natural solution that promotes healing. And it gets better, after the L-PRF clot is ready, it’s dipped in bone grafting material. So, we end up with a 100% biocompatible material that accelerates healing, as well as bone and gum formation. Pretty clever, huh?